"How do I create and manage my patient SOAP Notes?"
The Client SOAP Note tool allows you to document and monitor client treatment activities and progress. Notes can be recorded on each session and then reviewed before the next session.
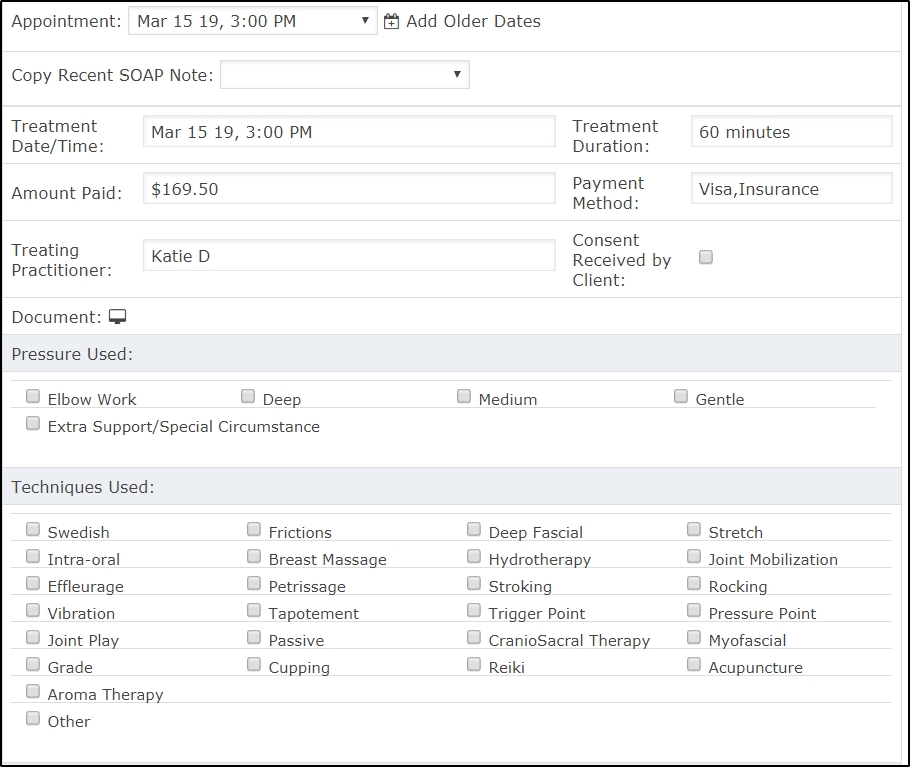
The tool provides a drop down list of recent client appointments, check boxes for techniques and areas treated, as well as 4 independent text boxes, one for each documentation (Subjective observations, Objective observations, Assessment and Plan).
Here's how SOAP Notes are created.
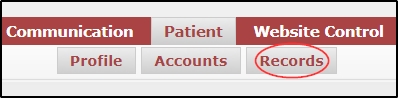
Navigate to Patient >>> Records
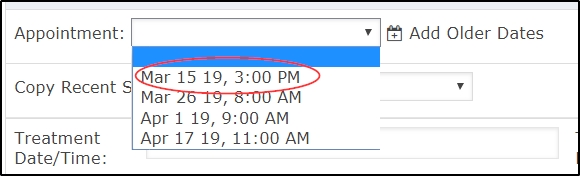
Select the appointment date from the drop down menu. Treatment Date & Time, Practitioner, and Duration will fill in automatically based on what is in the calendar, after the note is saved.
Next, use the consent, areas treated, and technique check boxes, then place your cursor in the appropriate text box in the SOAP section and enter your treatment notes and observations.
Once complete click the Save ![]() button .
button .
Your client SOAP notes are stored by client and then ordered by date. Click on the SOAP history tab to review past client treatment notes where they can be reviewed, edited and/or printed.